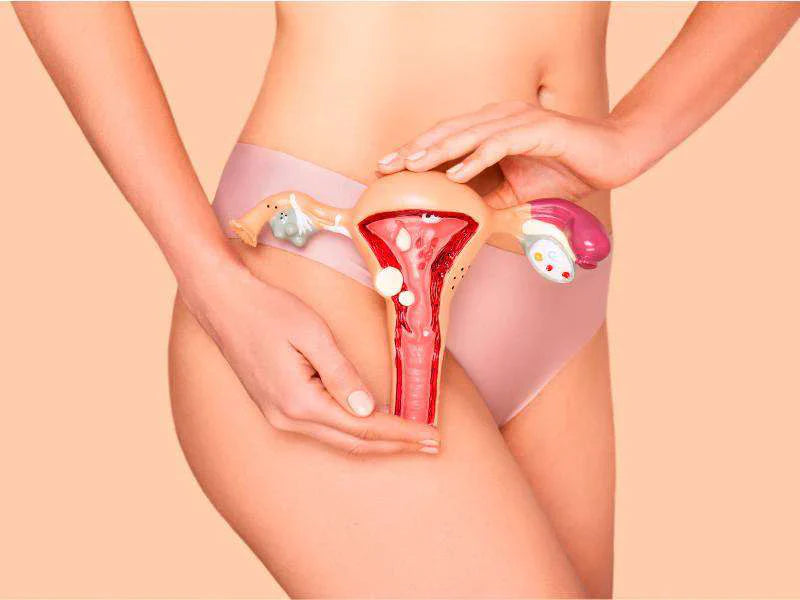
Don't panic! The discomfort you experience during menstruation is very common. It is what is known as pelvic pain, a condition that usually occurs in the lower abdomen. This pain is not always constant; it may come and go at different times. Its intensity also varies. For example, it may be experienced as mild discomfort in the pelvic area. In other cases, there may be intense, throbbing pain. If so, it can interfere with daily activities (MayoClinic, 2019a). It originates in the pelvic organs, which include the pelvis, uterus, vagina, rectum, and anus (MayoClinic, 2019a). This pain is primarily felt in the area below the navel, which includes the lower stomach, lower back, buttocks, and genital area (NIH, 2015). While pelvic pain is common during menstruation, in menopause and postmenopause, since you are no longer in the reproductive stage, it is not normal; it may be a symptom that something is wrong with your body (MayoClinic, 2019a). If this is your case, here we are going to tell you what can cause it and what to do to prevent it.
Causes of pelvic pain in menopause
Irritable bowel syndrome
Irritable Bowel Syndrome is one of the main causes of pelvic pain during menopause. Symptoms associated with this condition -such as bloating, constipation, or diarrhea- may be the source and pressure in this area causing the pain (MayoClinic, 2019b).
Pelvic Inflammatory Disease
Pelvic discomfort is also common. In this way, Pelvic Inflammatory Disease is caused by a complication from a sexually transmitted infection. Bacteria spread from the vagina to the uterus causing damage to all the surrounding tissue. In addition to pain, you may have other symptoms and signs such as abnormal vaginal discharge (heavy and foul-smelling); pain during intercourse; difficulty urinating; and bleeding (Johnson, 2020; MayoClinic, 2021a).
Ovarian cancer
Don't worry: having pain does not mean you have this type of cancer. However, you should be aware that it may be one of the causes. It is caused by an abnormal growth of ovarian cells that invade and destroy healthy tissues. It is a condition that is generally detected when it is already advanced because it does not cause any noticeable symptoms; when they appear, they are confused with other diseases. Signs include pelvic pain, unexplained weight loss, back pain, and changes in bowel habits, such as constipation and frequent urination (Mayo Clinic, 2021b).
Ovarian cysts
They are defined as an abnormal growth of tissue that develops when the ovaries are unable to release an egg. Cysts may cause swelling, pressure, or pelvic pain. Most are not cancerous and, in many cases, go away on their own; however, in other cases, a cyst may bleed or burst. This situation can cause acute and severe pelvic pain and require medical treatment (Johnson, 2020).
Endometriosis
Endometriosis occurs when the tissue that lines the inside of the uterus grows outside the uterus. It affects the ovaries, fallopian tubes, and the tissue that lines the pelvis, causing chronic and persistent pain in the area. This condition can also cause bleeding and swelling in the pelvis. Endometriosis can cause subsequent problems such as pelvic adhesions, which occurs when two tissues should not be connected in the first place. This can cause chronic pain as the body struggles to adapt to the adhesion (Johnson, 2020).
Urinary tract infections
If you see these problems regularly, you should know that this may be one of the causes. A urinary tract infection can also be another cause of pelvic pain. It happens when bacteria enter from the vagina into the bladder or other part of the urinary tract. The infection causes tissue inflammation and can lead to pain during urination and pelvic pain (Johnson, 2020; MayoClinic, 2020).
When to consult a physician?
At this point, you may be wondering when you should have a medical consultation. Well, if you are going through menopause and have pelvic pain, you should not ignore it. Ideally, you should see your doctor immediately for early diagnosis and treatment. You'll be much more relaxed if you do!
Warning signs
For example, in women with pelvic pain the presence of the following symptoms are alarm signals (Barad, 2020):
- Dizziness.
- Sudden loss of consciousness, even if brief.
- Fainting.
- Sudden state of shock.
- Vaginal bleeding after menopause.
- Fever or chills.
- A sensation of chronic and sudden pain.
- Nausea or vomiting.
- Excessive sweating.
- Feeling agitated for no reason.
- If you present one or more of these symptoms, you should seek medical advice immediately.
What to do to avoid pelvic pain?
Stay active
It may be hard to do, but physical activity increases blood flow and chemicals (known as endorphins) that make you feel good. These chemicals are the body's natural painkillers, and just 30 minutes of minimal physical activity a day can help prevent pelvic pain-causing diseases (Johnson, 2021).
Change habits
Did you know that changing a habit can also help control and prevent the pain? For example, if you smoke, you should quit. Nicotine can cause your nerves to swell and cause pain. If you are overweight, shedding a few pounds can reduce pressure on the nerves and therefore help relieve pain (Johnson, 2021; Barad, 2020).
Take supplements
Many times, pelvic pain is related to lower-than-normal amounts of vitamins and minerals. For example, deficiencies in vitamins D and E and magnesium can help you develop conditions that cause pain. Also, taking natural supplements such as licorice, dong quai, and evening primrose oil can help prevent inflammation and, therefore, pain-causing conditions. However, it is relevant that before deciding on these options you first consult your physician (Johnson, 2021; Barad, 2020).
Relax
Sometimes you need to take a break from your problems. Practicing meditation, yoga, and breathing techniques can help prevent pelvic pain. These techniques, especially yoga, can help prevent you from developing diseases that cause pelvic pain. In addition, they can decrease stress, increase a sense of well-being and help you sleep better (Cronkleton, 2021).
Take care of your diet
What you eat can influence the development of diseases that cause pelvic pain. For example, including more fiber in your diet can be beneficial. Also, foods that are rich in fatty acids (such as omega-3 found in salmon and chia seeds) and antioxidants (found in fruits, such as strawberries, oranges, lemon, melon, and plum; and green leafy vegetables such as spinach and broccoli) can be very beneficial. Conversely, you should avoid eating a diet high in trans fats and high in red meat or gluten (Olsen, 2020).
See your doctor regularly
Finally, some chronic conditions such as arthritis can cause you to develop pelvic pain. Therefore, you should see your doctor regularly. This may be the best way to prevent and identify diseases and conditions early (Seladi-Schulman, 2020). You already know that menopausal pelvic pain can be the result of a condition with a wide range of causes. You should always consult your doctor if you experience this type of pain, especially if it occurs regularly and with sexual intercourse. Together you can probably run tests to find out the cause and treat it appropriately.
References
Barad, D. (2020). Dolor pélvico. Manual MSD: Versión para profesionales. https://www.msdmanuals.com/es-co/professional/ginecolog%C3%ADa-y-obstetricia/s%C3%ADntomas-de-los-trastornos-ginecol%C3%B3gicos/dolor-pelviano Cronkleton, E. (2021).
Yoga for endometriosis: try these stretches to relieve pain. Healthline. https://www.healthline.com/health/fitness/yoga-for-endometriosis Johnson, J. (2020).
¿Qué causa el dolor pélvico en las mujeres? Medical News Today. https://www.medicalnewstoday.com/articles/es/dolor-pelvico-en-las-mujeres Johnson, T. (2021).
6 ways to ease your chronic pelvic pain. WebMD. https://www.webmd.com/women/guide/ease-chronic-pelvic-pain MayoClinic. (2019a).
Síntomas. Dolor pélvico. Causas. Mayo Clinic. https://www.mayoclinic.org/es-es/symptoms/pelvic-pain/basics/causes/sym-20050898 MayoClinic. (2019b).
Dolor pélvico crónico en mujeres. Mayo Clinic. https://www.mayoclinic.org/es-es/diseases-conditions/chronic-pelvic-pain/symptoms-causes/syc-20354368 MayoClinic.(2020).
Infección de las vías urinarias. Mayo Clinic. https://www.mayoclinic.org/es-es/diseases-conditions/urinary-tract-infection/symptoms-causes/syc-20353447 MayoClinic. (2021a).
Enfermedad inflamatoria pélvica IEIP). Mayo Clinic. https://www.mayoclinic.org/es-es/diseases-conditions/pelvic-inflammatory-disease/symptoms-causes/syc-20352594 MayoClinic. (2021b).
Cáncer de ovario. Mayo Clinic. https://www.mayoclinic.org/es-es/diseases-conditions/ovarian-cancer/symptoms-causes/syc-20375941 MedlinePlus. (2020).
Dolor pélvico. MedlinePlus: Biblioteca Nacional de Medicina. https://medlineplus.gov/spanish/pelvicpain.html NIH. (2015).
Dolor pélvico: información sobre la enfermedad. National Institute of Child Health and Human Development. https://espanol.nichd.nih.gov/salud/temas/pelvicpain/informacion Olsen, N. (2020).
What to eat and what to avoid if you have endometriosis. Healthline. https://www.healthline.com/health/endometriosis/endometriosis-diet#foods-to-avoid Seladi-Schulman, J. (2020).
Pelvic pain when walking: 9 common causes. Healthline. https://www.healthline.com/health/pelvic-pain-when-walking#prevention
You May Also Like

JOIN US AND GET 10% OFF
Sign up to our newsletter to access free resources, advice and support.