Did you know that at least three out of four women have had a vaginal fungal infection at some point in their life and that menopause can increase the risk of having these infections? (Mayo Clinic, 2021). Here's everything you need to know about vaginal yeast infections. How they happen, how they are treated and, of course, how you can prevent them.
What is a vaginal fungal infection?
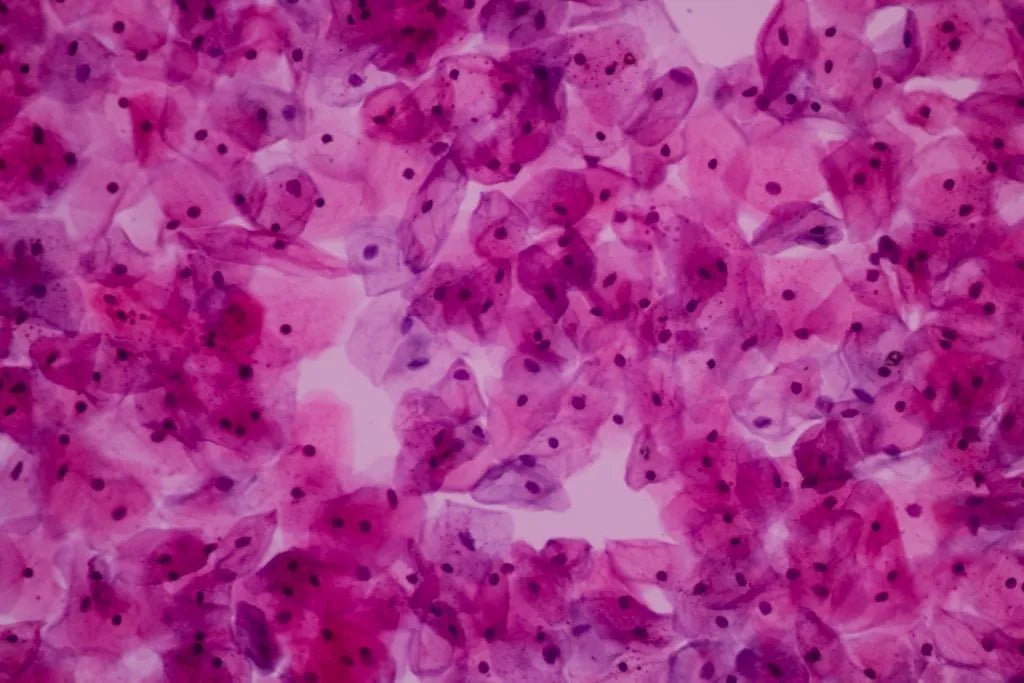
The vaginal fungal infection, also called vaginal candidiasis, occurs when a fungus, commonly candida albicans, infects the inside of the vagina (Willems et al., 2020). It is important to emphasise that this fungus is a normal occurring fungus which inhabits the human microbiome. It only becomes a problem when the body is unable to control its growth and reproduction. When that happens, it is usual that it infects the vagina, although it can also be in:
- Mouth
- Throat
- Even the skin (Willems et al., 2020).
Why do fungal infections appear in menopause?
Your vagina normally has a mixture of microorganisms inside it. For example, bacteria such as lactobacillus and fungi such as candida. In normal conditions, these are in perfect balance so that they do not produce symptoms or discomfort. Lactobacilli are found in greater proportion, and their function is to make the vagina acidic. That, in turn, prevents the overgrowth of the fungi (Willems et al., 2020). However, when an imbalance occurs, they begin to grow uncontrollably, invading the vagina and giving rise to Fungal infection (Willems et al., 2020). During menopause, a decrease in oestrogen hormones circulating in the blood occurs. It has been evidenced that this causes the normal flora of the vagina to be altered, in addition to:
- Decreasing the number of lactobacilli
- Increasing the risk of bacteria and fungi growing out of control (Kim et al., 2017).
Risk factors
As we have mentioned, the mere fact of being a woman already makes you prone to having a vaginal fungal infection; even more so if you are in menopause. However, there some factors can increase the risk of suffering from this disease. Among them are the following (Goje, 2021):
- Use of antibiotics: antibiotics can sweep away the protective bacteria from the vagina.
- Uncontrolled diabetes: people with diabetes and poor blood glucose control are more likely to get thrush.
- Impaired immune system: any condition that weakens the immune system, such as HIV or cancer, favours candidiasis. This is because the body cannot fight the infection.
- Use of an intrauterine device as a contraceptive method.
Signs and symptoms of fungal infection
A vaginal fungal infection can occur differently in each woman. Some have little discomfort, while others have all the symptoms. The most common symptoms are (MedlinePlus, 2019):
- Abnormal discharge of white colour and thick texture.
- Redness of the vulva and vagina area.
- Itching or irritation in the vulva, like those of vaginal atrophy.
- There may also be a rash in the genital region.
- It rarely causes pelvic pain or vaginismus (which is a painful spasm of the vagina).
Overview of its diagnosis and treatment
Signs and symptoms are quite characteristic of the disease and will guide a doctor or pharmacist to diagnose the condition. However, a urine sample is sometimes taken to confirm the condition. This step is important to rule out other classes of vaginitis, such as that caused by bacterial infections or parasites (Goje, 2021). Infections of this type usually respond very well to antifungal drugs of topical origin applied by vaginal creams, eggs, or gels. In some instances, there can be complications, such as (Mayo Clinic, 2021):
- When it appears in pregnant women, people with diabetes, or HIV.
- If the cause is a uncommon fungus.
- In case of severe signs and symptoms such as extreme redness with tears, sores, or cracks of the skin.
- When it becomes recurrent, with four or more episodes per year.
In these cases, the treatment is usually more extensive. It may even involve the use of oral antifungal medications (Mayo Clinic, 2021; Goje, 2021; Willems et al., 2020).
How to prevent fungal infection in menopause?
You can prevent vaginal fungal infections with simple intimate care habits (Mayo Clinic, 2021):
- Clean your genital area with warm water and mild products.
- Use vaginal cleansers that help to preserve the acidity in the area.
- Avoid douching, heavily scented intimate products, sanitary napkins, or tampons.
- Wear cotton underwear.
- Do not stay in wet clothes (swimsuit or gym sets) for a long time.
- Only take antibiotics when necessary for the presrcved time length.
Vaginal fungal infection is a common problem in women, no matter their age. It usually causes localised discomfort in the vagina, but fortunately, they usually improve with topical treatment. Best of all, you can prevent this infection with basic hygiene measures that are effective even during menopause.
References
- Goje, O. (2021, April). Vaginal yeast infection (candidiasis). Manual MSD. https://www.msdmanuals.com/es-ve/hogar/salud-femenina/infecciones-vaginales-y-enfermedad-inflamatoria-p%C3%A9lvica/infecci%C3%B3n-vaginal-por-levaduras-candidiasis
- Kim, J.M., and Park, Y.J. (2017). Probiotics in the prevention and treatment of postmenopausal vaginal infections: review article. Journal of menopausal medicine, 23 (3), 139–145. https://doi.org/10.6118/jmm.2017.23.3.139
- Mayo Clinic. (2021, December 14). Vaginal candidosis. https://www.mayoclinic.org/es-es/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999
- MedlinePlus. (2019, June 30). Vaginal candidosis. https://medlineplus.gov/spanish/ency/article/001511.htm
- Willems, H., Ahmed, S.S., Liu, J., Xu, Z., and Peters, B.M. (2020). Vulvovaginal candidiasis: a current understanding and burning questions. Journal of Fungi (Basel, Switzerland), 6 (1), 27. https://doi.org/10.3390/jof6010027
You May Also Like

JOIN US AND GET 10% OFF
Sign up to our newsletter to access free resources, advice and support.














